Interesting!!! Nuff said about this one.
'via Blog this'
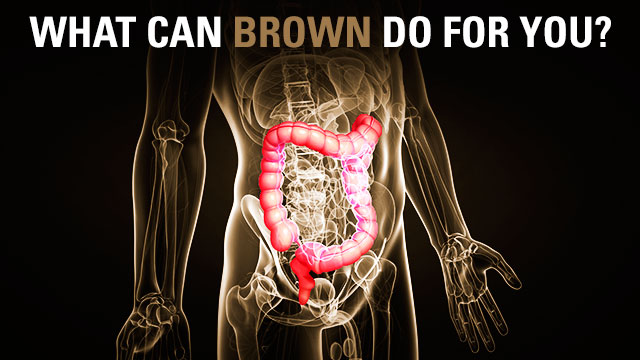
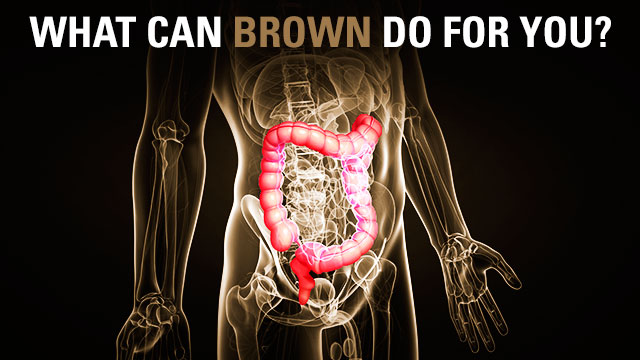
Fecal transplants cure diarrhea, modulate testosterone levels
Nutella was not used as a placebo control.
From some perspectives, we humans aren't really so much individuals as we are walking ecosystems—our bodies carry more bacterial cells—with their own genomes and agendas—than the total count of human cells we're composed of. Bacteria cover our skin, get to our food before we have the chance to absorb it, and in many cases stay helpfully out of the way of the immune system.Given all that, it shouldn't be a surprise that we're finding that bacteria can have significant effects on the human body in ways that go well beyond causing an infection. Two articles that appeared this week drive that home. In one, doctors cured a recurring, diarrhea-causing infection simply by transplanting gut bacteria from a healthy individual. And in the second, the bacterial transplants altered the progression of type 1 (autoimmune) diabetes in mice—by altering the animal's testosterone levels.
Fighting bacteria with bacteria
Clostridium difficile, or C. diff, is a bacteria that tends to cause extended bouts of diarrhea. In about 20 percent of the cases that end up under a doctor's care, it will get into the digestive system and refuse to come back out, creating recurring bouts of illness that don't respond to most antibiotics. At that point, the standard of care is an intensive course of vancomycin, which only works in about 60 percent of patients. With each further recurrence, the rate of success goes down even further.
Anecdotal evidence and case reports had suggested that the problem wasn't so much the presence of C. diff as the fact that it had grown out of balance with the rest of the gut's bacterial ecosystem. To get the gut back into balance, fecal transplants had been tried and, anecdotally at least, they worked. So some doctors in the Netherlands decided to do a clinical trial, comparing a fecal transplant to standard care with vancomycin. The trial was what the researchers called "open label," meaning that people were aware they were having a feeding tube stuffed down their nose to deliver someone else's poop into their body. (A Twitter pundit suggested a Nutella infusion might make for a good placebo control.)
A few dozen healthy volunteers were screened for a huge panel of infectious diseases, and those who came through clean were asked to rush their bodies' first deliveries of the day to the hospital, where it was mixed with saline and had the particulates removed. The results then went into the gastro-nasal tube, given to patients after their original gut flora had been cleared out by a "bowel lavage."
The authors had originally planned to get 40 patients for each group, but the fecal transplants were so successful, they stopped the trial after only 16 patients had received a transplant. Of these, 13 (80 percent) were cured after a single transplant. Two of the remaining three were cured after their second, bringing the success rate up to over 90 percent. In contrast, the success rate of vancomycin treatments was down around 30 percent.
The biggest problem? Enrolling patients. Most people who agreed to participate in the trial only did so after conventional treatments failed several times, "reflecting the reluctance of patients and physicians to choose donor-feces infusion at an early stage."
Bacteria, sex, and immunity
It's easy to view this as a demonstration of the hygiene hypothesis, which posits that all sorts of health issues are linked to exposure to a variety of infectious agents, which the immune system then learns to live in harmony with. But a second paper appeared this week that cautioned against viewing things as being quite that simple.
The paper focused on the progression of type 1 diabetes, which is the product of an autoimmune attack on the insulin-producing cells. There's a special strain of mice, called NOD (for non-obese diabetic) that are prone to developing this disorder. The mice show properties that are very much like the human version of the disease: it's genetically complex, the progression is influenced by environmental factors, and it strikes females more severely than males.
And, unexpectedly, it's influenced by gut bacteria. There was some hint of this, given that other researchers had shown that a systematic exposure to bacterial proteins was able to suppress the development of the disease. But the authors found an unexpected effect when they tested how the disorder progressed in mice raised in germ-free conditions. Rather than accelerating the development of symptoms in all mice, the germ-free conditions accelerated the progression in males, making them (at least in this assay) indistinguishable from females.
So the researchers tried an experiment: they took germ-free NOD mice and did a fecal transplant from adult male animals (mice are naturally coprophagic, so the mice took a lot less convincing than did the humans). When female NOD mice received gut bacteria from males, it actually slowed the disease progression down. The apparent sex difference in autoimmune function was mediated in part by gut bacteria.
Your first thought might be that testosterone in males could create a different environment in the gut, causing it to host a different diversity of species. It's a reasonable guess, but it's wrong. Instead, the researchers found that the transplant of gut bacteria caused a surge in testosterone production by females that lasted for up to 14 weeks. This had no effect on the female's fertility, but it did clearly alter immune function. If the authors injected these mice with a testosterone inhibitor, the diabetes protection went away.
All of which indicates that the other intuitive idea—that gut bacteria influence immune function by interacting directly with immune cells—also can't be right, or at least can't be everything. Clearly, the production of testosterone, by whatever cells may be producing it, plays a key role.
Although the papers argue against some of the simpler views of human health—bacteria are all bad, or not having exposure to pathogens means an overactive immune system—they both argue that viewing our bodies as a complex ecosystem can help provide insight into human health.
New England Journal of medicine, 2013. DOI: 10.1056/NEJMoa1205037 and Science, 2013. DOI:10.1126/science.1233521 (About DOIs).
Fecal transplants cure diarrhea, modulate testosterone levels | Ars Technica:'via Blog this'
